Medicare Member Enrollment Technology
A comprehensive technology solution for the Medicare member enrollment administration.
The enrollment process can be laden with pain points especially when it comes to eligibility verification, enrollment acceptance and validation, and benefit activation and notification. And each step is bound by federal regulations, making compliance paramount.
Insert a built-for-Medicare enrollment solution that supports the entire enrollment lifecycle with ease and a focus on your member’s experience.
Tailored for Medicare enrollments
This purpose-built system is meticulously crafted to cater specifically to the complexities of the Medicare landscape. Unlike generic solutions, our Miramar:Member has evolved over time to meet the exacting standards set by CMS, adapting to stringent guidelines, service level requirements, and industry compliance measures.
Benefits of the enrollment solution
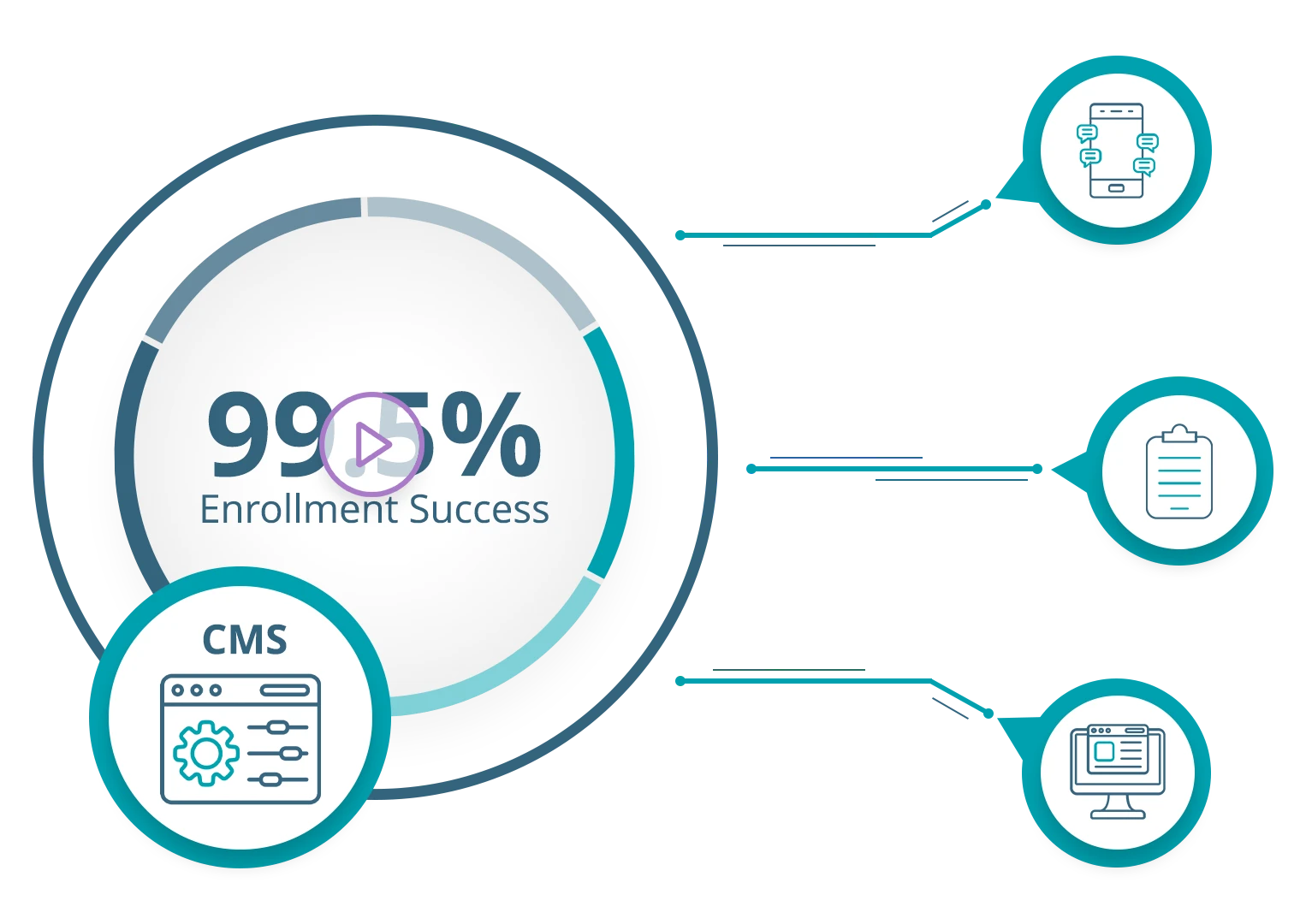
Multi-Channel Enrollment Management
Experience streamlined intake and verification processes across various channels, ensuring data accuracy and completeness while reducing rejections
Real-Time Work Queue Distribution
Tasks are efficiently allocated in real-time, enhancing productivity and responsiveness.
Automatic Triggers and Configurable Workflows
Benefit from automatic triggers for exhibits upon enrollment and TRR processing, alongside configurable workflows tailored to member enrollment status.
Timely Reconciliation and Integration
Enjoy timely and accurate reconciliation through automated processes, coupled with full integration with premium payment information to promptly address member needs.
CMS Compliance
We capture all CMS-mandated information and update the platform, maintaining your compliance with evolving Medicare regulations, reducing risk, and ensuring quality.
Key functionality of our Medicare member enrollment management solution
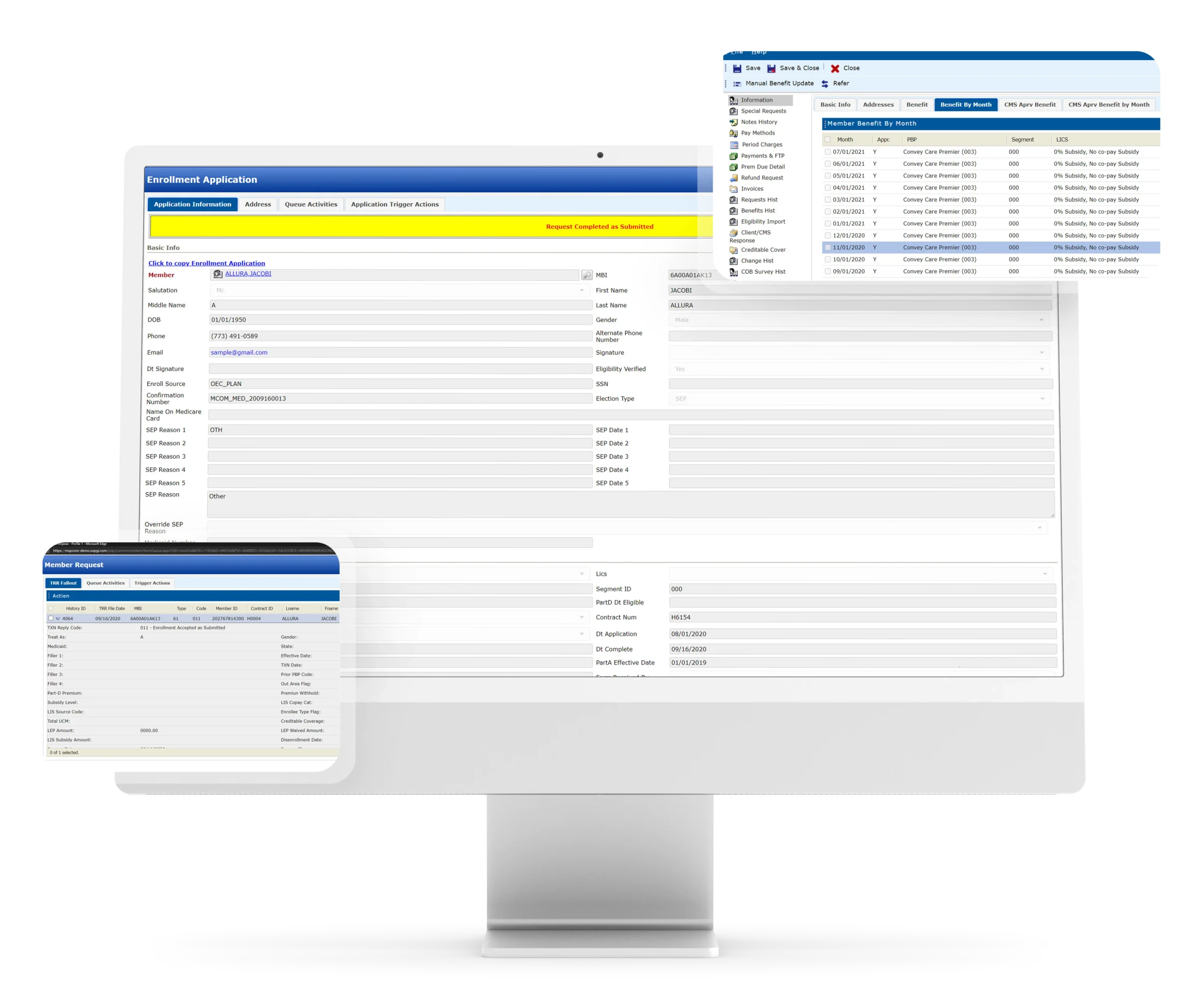
Enrollment Intake
Disenrollment Processing
Cancellation Processing
LEP Attestation Processing
CMS Reconciliation
-
- Member Eligibility
- Member Demographics
- LIS Status
- Enrollment Penalty
Broker Commission Data Feed
Eligibility Verification (BEQ)
Enrollment Verification
Opt-Out Processing
Out of Area Processing
Telephonic Pre-enrollment and Enrollment
-
- Marketing Campaign Tracking
Work Queues
Enrollment Processing
Eligibility Processing for Employer Groups
Retro Processing
TRR Processing
Medical Claims Eligibility Feed
PBM Eligibility Feed
Exhibit Triggering
Enrollment Maintenance
Incomplete Enrollment / Disenrollment Review
Good Cause Reinstatements
BAE / LIS Override
PBM Reconciliation
-
- Member Eligibility
- LIS Status
- Member Demographics
SmartWizards
Take the first step toward seamless Medicare enrollment management.
Our team of experts is standing by to show you the difference a purpose-built solution can make and how you can revolutionize your operations.
