Your Medicare Plan, Optimized

Empowering health plans across the member lifecycle since 2001
Streamline operations, secure compliance, and elevate the member experience.
Convey Health Solutions is a leading provider of technology and services for Medicare plans. With a deep understanding of the complexities of the Medicare market, Convey offers a suite of solutions that span the entire plan and member lifecycle.
We help your MA / MAPD, PDP, and/or EGWP organization navigate the intricacies of Medicare.
Simplify complex member relationships
Improve operational efficiency
Drive compliance and quality
Medicare Advantage Plans
(MA / MAPD)
Whether your health plan is seeking a technology-only solution, a comprehensive technology and service model, or expert advisory services, we work with you to develop the most cost-effective and compliant solution for your plan type:
- Health Maintenance Organizations (HMO)
- Preferred Provider Organizations (PPO)
- Medicare-Medicaid Plans (MMP)
- Program of All-Inclusive Care for the Elderly (PACE)
- Special Needs Plans (SNP)
• Including ISNPs, DSNPs, and CSNPs - Private Fee-For-Service Plans (PFFS)
- And more


Individual Prescription Drug Plans (PDP)
With high fixed costs, low margins, and an intensive regulatory environment, the Medicare Part D market is a challenge for any health plan. Having participated in Medicare Part D since its inception, Convey combines purpose-built technology, an experienced Part D service organization, and CMS-compliant processes to rapidly respond to the demands of the Part D market and population.
Our dedicated compliance and quality teams partner with your team to guarantee:
As a Pharmacy Benefit Managers (PBM) you may be assuming the role of Plan Sponsor. If so, you are often challenged to meet the needs of your clients with existing technology and services. Today, Convey Health Solutions serves some of the leading PBM providers. With Convey as your partner, you can select from a variety of services and solutions in order to meet the demands of your clients and the market.
Employer Group Waiver Plans (EGWP / MA-EGWP)
The Medicare Employer Group Waiver (EGWP) market is one of the most challenging markets within Medicare. Besides having to manage in a highly regulated environment, your plan must also face complex group-specific requirements that can create risk and add layers of manual processes and workarounds.
Traditional EGWP solutions combine multiple technologies and services that can cause disconnected processes and poor responsiveness.
Convey provides a fully integrated, single platform and service model to enhance your EGWP administrative program and deliver optimal service levels and higher member satisfaction scores.
Our EGWP solutions and services manage groups of any size or scale and serve some of the largest, most complex EGWP programs in the industry today.

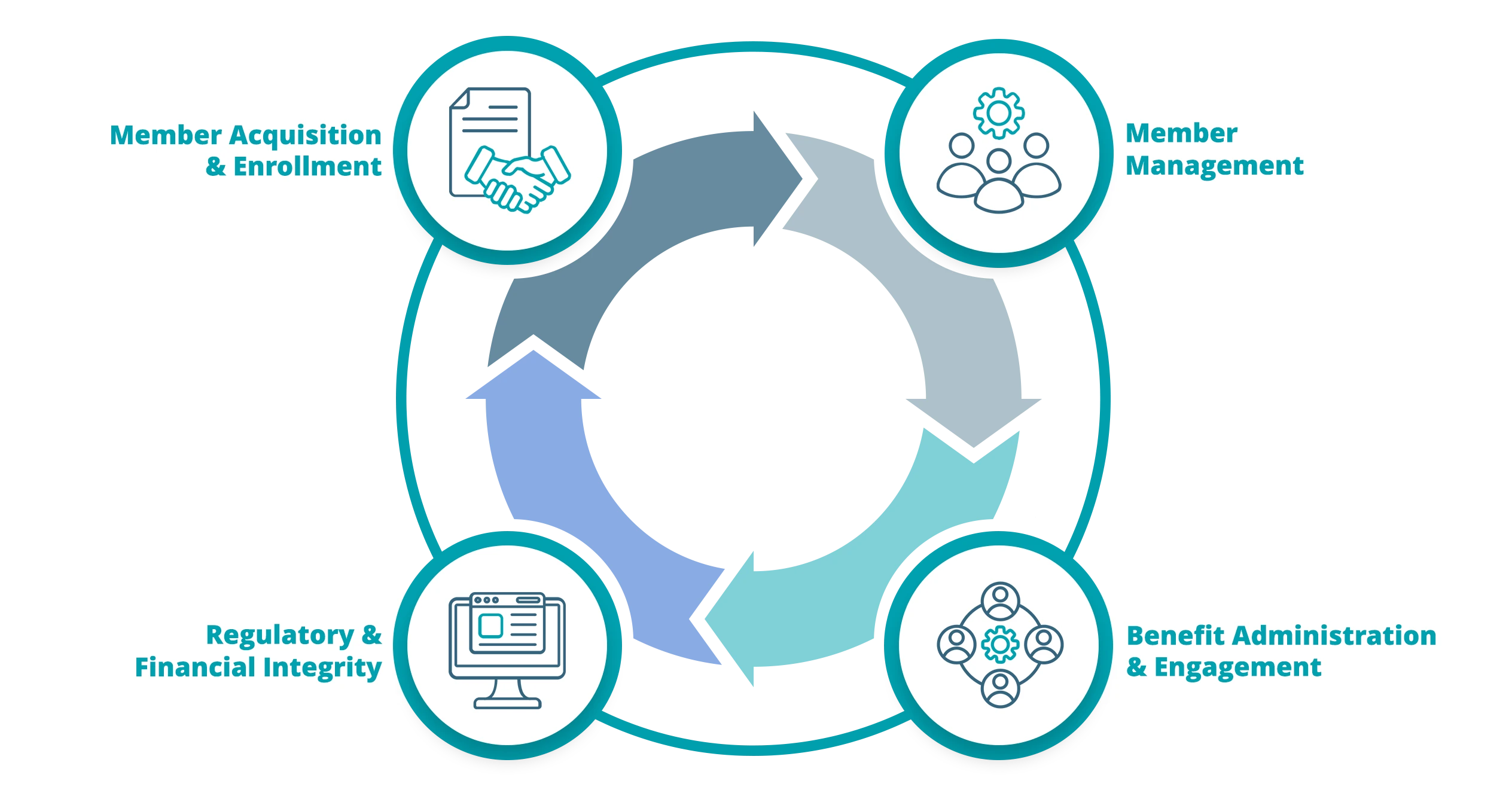
Optimize your Medicare plan and member lifecycle
Let’s partner to address the uniqueness and complexity of your plan and membership to improve efficiency, reduce costs, and enhance experiences in the following areas.
Member Acquisition and Enrollment
- Agent and Broker Management: Support for agent and broker networks, facilitating member acquisition.
- Eligibility and Enrollment Processing: Convey’s technology streamlines eligibility verification and enrollment processes, ensuring accuracy and efficiency.
- Member Onboarding: Improve member confidence in understanding your plan to drive CAHPS improvements and minimize grievances, complaints, and appeals.
Member Management
- Premium Billing and Payment Processing: Automated premium billing and payment processing, reducing errors, and improving cash flow.
- Customer Service: Highly trained customer and member services drive first-contact resolution for positive member experiences, improved satisfaction, and delight.
- Document Management: Efficient management of member documents, ensuring timely and accurate communication.
- Value Based and Payment Accuracy: Support of value-based care models and accurate payment processing.
- Appeals and Grievances Processing: Streamline the appeals and grievances process for timely resolution and member satisfaction.
Benefit Administration and Engagement
- Flex Card Programs: Allows members to use a benefit card to access extra benefit funds, simplifying the process of paying for healthcare costs.
- OTC Benefit Programs: Managed program for member’s access to non-prescription health and wellness products.
- Reward and Incentive Programming: Provide healthy rewards for healthy behaviors and engagement in healthcare management to improve business outcomes and increase member delight.
- Member Communication: Deploy coordinated and orchestrated communications to demonstrate you know the member, creating member trust and retention.
Regulatory and Financial Integrity
- Compliance Oversight: Monitor and ensure compliance with applicable state and federal laws and regulations, minimizing risks
- Membership and Financial Reconciliation: Robust reconciliation solutions to ensure accurate membership data and financial reporting
- Risk Adjustment and Suspecting: Accurate risk adjustment coding, suspecting, and analysis processes to ensure appropriate reimbursement for health plans.
Work with us