Over-the-Counter (OTC) Benefit
Convey’s integrated, end-to-end OTC benefit administration solution delivers the OTC solutions your health plan and members appreciate. We’ve been administering our comprehensive OTC benefits program since 2008.

Our position as a market-leading provider of supplemental OTC benefit administration services was built on the powerful combination of our proprietary Miramar technology and award-winning customer service. By managing member experience, compliance, and utilization, Convey reduces the burden and expense of your in-house program. Freeing up resources for your health plan’s fundamental and strategic priorities.
Member-centric design
Everything you and your members need for a successful supplemental OTC benefit program relies on keeping the member at the center.
Offer your members what they want and realize the benefits for your plan–a convenient benefit card, a catalog of OTC products available for home delivery, seamless integration with your reward and incentive programs, and clinical and chronic condition program alignment.


Integrated OTC benefit technology
The Miramar:Benefits platform is built for the management of supplemental benefits. It ingests your member data, empowering both our advocates you’re your members to navigate the OTC benefit program with ease. Because of this, we fully support and manage the program on your behalf:
- Flexible, configurable benefit design
- Comprehensive CMS and plan required reporting
- Eligibility file processing, from all formats
- Member interaction and benefit tracking
- OTC member website and mobile application hosting
- Shipping, mailing, app, web, merchant, and dialer integration
- Role-based security measures
OTC benefit card
The Convey OTC benefit card solution is a focal point of our member-centric OTC services. Our OTC benefit card program is designed to help your Medicare Advantage members achieve or maintain wellness by maximizing their OTC benefits and simplifying access to even more than their OTC benefit with integration into our flex wallet program.
Easy access
Member OTC benefit cards have a pre-determined allowance for approved, health-related OTC products. Items like cold or allergy medications, compression socks, and sleep aids are available in-store and through our home delivery program.
Our program provides you with a health plan branded website with live chat, a mobile app for 24/7 access, and a dedicated member contact center.
Comprehensive administration
Miramar:Benefits accommodates varying benefit designs and handles critical administrative functions, including:
- Business rules management
- Transaction activity and account balance access for members and plans
- Benefit utilization monitoring
- Disease-state programming
- Member and plan self-service functionality
- Fulfillment services
Expanded benefit options
Convey’s flexible card solution supports nearly all supplemental benefits (50 purses). From the must-haves (dental, vision, and hearing) to wellness, transportation, safety, fall prevention, and connected devices.
With one benefit card, your members can access all integrated benefits and merchants via in-store purchases, home delivery, curbside pickup, and in-office transactions. And one award-winning customer service center coordinates it all.
Your plan has one account manager, one reporting suite, one set of service-level agreements, and consolidated billing.

Secure and compliant
Our compliance and technology teams ensure that our operations and IT systems (HIPAA, PHI, PCI, Privacy, and Security) are properly maintained and focused on upholding all regulatory requirements. Convey works with your compliance team to make certain the program meets your internal quality assurance policies.
We hold HITRUST certification for information security and adhere to the Seven Fundamental Elements of an Effective Compliance Program (OIG).
Our data-driven results
Data analytics uncover opportunities to improve members’ clinical benefits and elevate the member experience. Valuable insights can be gained when plans examine member cohorts and conditions and evaluate initiative overlap.

Connect benefit and claims data, demographics, and CMS risk scores
Finding: With Convey’s implemented CMS risk adjustment model, we uncovered that members using our OTC benefit program trended better over time for many member cohorts and conditions.
Want to know more about how the use of your supplemental benefit programs can lead to reduced costs?

Link member interaction and care program effectiveness
Medicare Advantage member interactions are high when managing supplemental benefit programs. Introducing care programs and offering incentives for participation present great opportunities.
Finding: Members who use the OTC benefit were found to overlap with documented participation in clinical programs in place with their health plan.
Ask us about our award-winning member services.
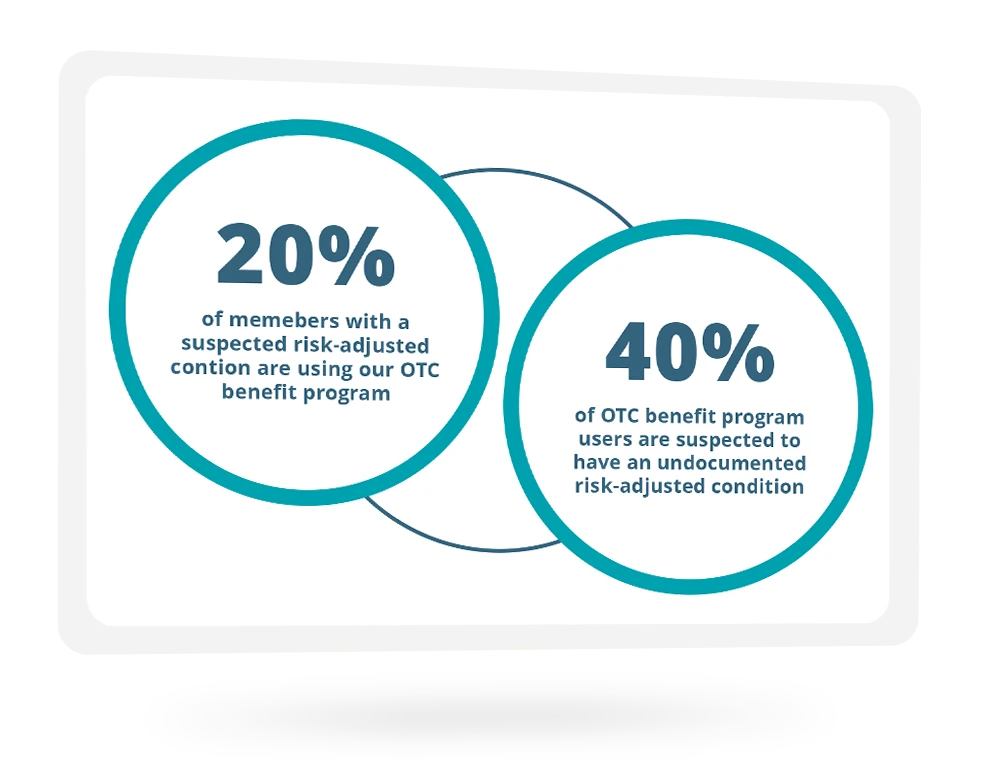
Uncover risk gaps through member activity
Findings: Whether previously suspected of certain conditions or not, specific purchasing or utilization behavior can identify potential risk gaps and intervention opportunities or confirm self-care.
For example, certain high-quantity product purchases can indicate substance abuse. Those who purchase diabetic supplies such as alcohol prep pads and diabetic socks can be identified as managing their diabetes or as unknown diabetics.
Interested in how to uncover this within your membership?
