Look to features to support the plan and member experience like advanced reporting, seamless access to benefits, and comprehensive support services
As we move further into 2025, I’m energized by the strategic conversations we’ve continued having with our Medicare Advantage clients. These discussions—reflecting on the recent Annual Enrollment Period (AEP) and looking ahead to the 2026 plan year—have reinforced why we’ve expanded our solution suite and strengthened our commitment to innovation and service.
I am excited to share significant enhancements to our 2025 supplemental benefits program. These updates are not just about adding new features; they represent our unwavering commitment to elevating the plan and member experience through advanced reporting, seamless access to benefits, and comprehensive support services.
Why We Reimagined Our Supplemental Benefits Platform
In a recent discussion with our product team, they emphasized the core philosophy driving these enhancements. Our 2025 supplemental benefit program reflects our dedication to improving the member experience through innovation, transparency, and flexibility. We are proud to offer a member-centric platform that complies with today’s regulatory requirements and simplifies the benefits experience. Our clients are equipped to support the diverse needs of plan members.
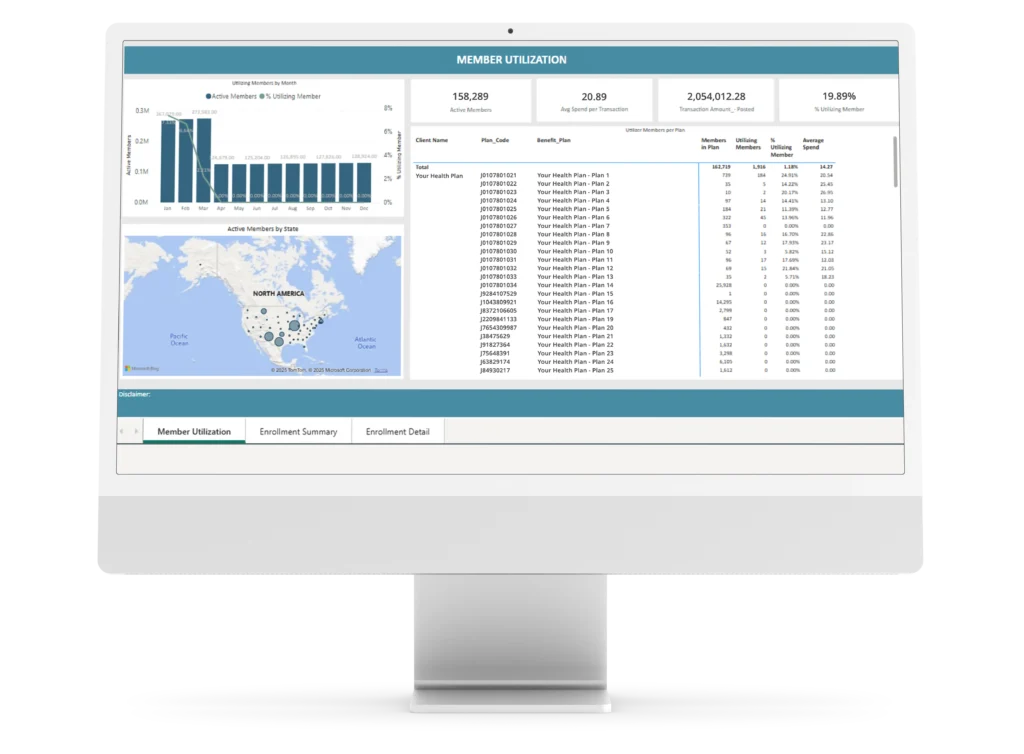
New features in this year’s program include advanced reporting capabilities, such as accessible CMS-required encounter data and a self-service administrative portal tailored for health plan product managers and leaders. This empowers our clients with the flexibility, tools, and features necessary to thrive in today’s dynamic healthcare environment.
We’ve also expanded the benefit card’s merchant network, offering members a broad range of redemption options across various benefit categories. This innovation ensures that members have easier access to essential services such as over-the-counter (OTC) products, nutrition, transportation, personal emergency response, and hearing.

A Strategic Vision for Growth, Innovation, and Member-Centered Care
In a conversation with Dan Finke, our chief executive officer, he shared his vision for the future: “At Convey, we are committed to providing health plans with the solutions and tools to succeed within a highly regulated Medicare environment. Our expanded offering and capabilities are a reflection of our ongoing efforts to support our clients in providing more personalized, seamless experiences for their members.”
As we continue to lead the way in providing comprehensive technology-driven solutions for health plans, our integrated member services platform ensures that health plans and their members have the tools, resources, and ongoing support needed for success. In addition to enhanced member support, our innovative flexible benefit card enables in-person redemption, while home delivery services for benefit-related products ensure a seamless, convenient experience for all beneficiaries.
As we look to the future, we remain dedicated to fostering partnerships that drive growth and innovation, ensuring that our clients are well-equipped to help members access and use benefits. We are excited to continue these strategic conversations and explore new opportunities to enhance our solution suite for the benefit of all.
To learn more about our enhanced supplemental benefits program and how it can benefit your health plan, contact us today to schedule a personalized consultation.
About Convey Health Solutions | Convey Health Solutions is a specialized healthcare technology and services company that is committed to providing clients with healthcare-specific, compliant member support solutions utilizing technology, engagement, and analytics. The company’s administrative solutions for government-sponsored health plans help to optimize member interactions, ensure compliance, and support end-to-end Medicare processes. By combining its best-in-class, built-for-purpose technology platforms with dedicated and flexible business process solutions, Convey Health Solutions creates better business results and better healthcare consumer experiences on behalf of business customers and partners. The company’s clients include some of the nation’s leading health insurance plans and pharmacy benefit management firms. Their healthcare-focused teams help several million Americans each year to navigate the complex Medicare Advantage and Part D landscape. To learn more, please visit www.ConveyHealthSolutions.com.

