Medicare Member Management


Do you have the necessary holistic approach to your members’ entire journey with your plan?
Our built-for-purpose platform is constructed to master complex processes for health insurance enrollment, premium billing, document processing, and more.
Convey’s Miramar:Member Platform
Delivers flexible business process solutions for the operational results and member experience you strive for.
Comprehensive Medicare Member Management
Enrollment & Reconciliation
Full member enrollment management, from intake and verification to reporting back to your health plan.
Billing
Complete member eligibility, invoicing, and payment processing of plan premiums.
Document Processing
Effortless document capture and fulfillment including document triggering integrations.
Grievance Management
Comprehensive analysis of the underlying causes of every grievance type.
Customer Service
Address member needs with dynamic member services and customer experience technology.
Enrollment & Reconciliation
Keep your health plan members happily enrolled. From intake and verification to reporting, Miramar offers total member enrollment management with automated and accurate reconciliation processes.
Need a standalone reconciliation solution?
Eliminate missed revenue and inaccurate claims payments. Our Miramar:Reveal solution increases visibility into how data flows through your organization and ways to improve operational success.
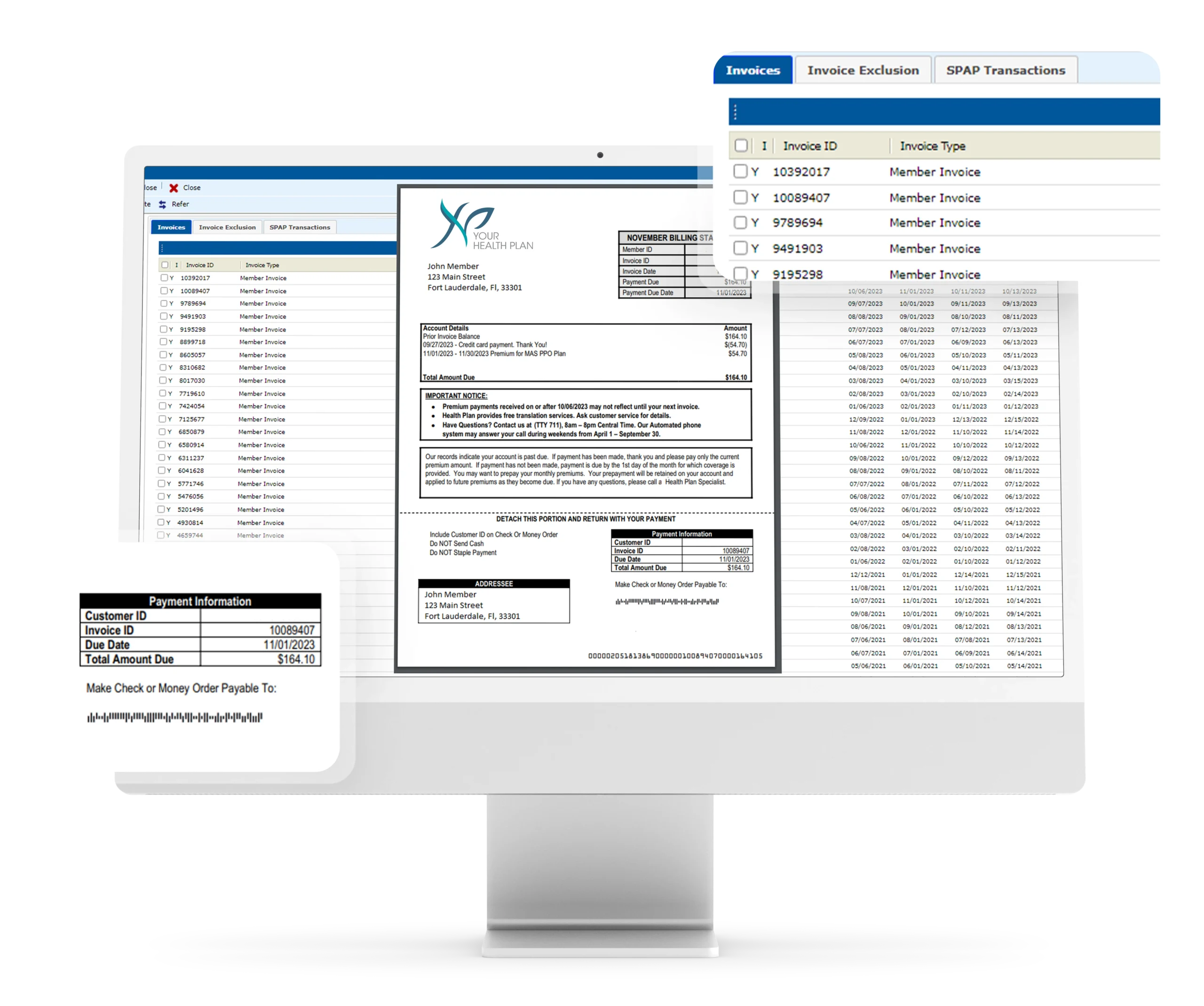
Premium Billing
Experience the power of automated adjustments for member coverage changes. Unlock personalized invoicing, versatile payment options, and seamless integration with premium payment information, empowering you to promptly meet the ever-changing needs of your members.
Document Processing
Extensive document capture and fulfillment services linked to every stage of the Medicare pre-enrollment and enrollment process, including seamless integration of document triggers for all enrollment, billing, and grievance procedures.
Grievance Management
Deliver a detailed root cause analysis for every type of grievance, and kickstart a series of improvements to effectively alleviate long-term grievances while enhancing customer satisfaction.
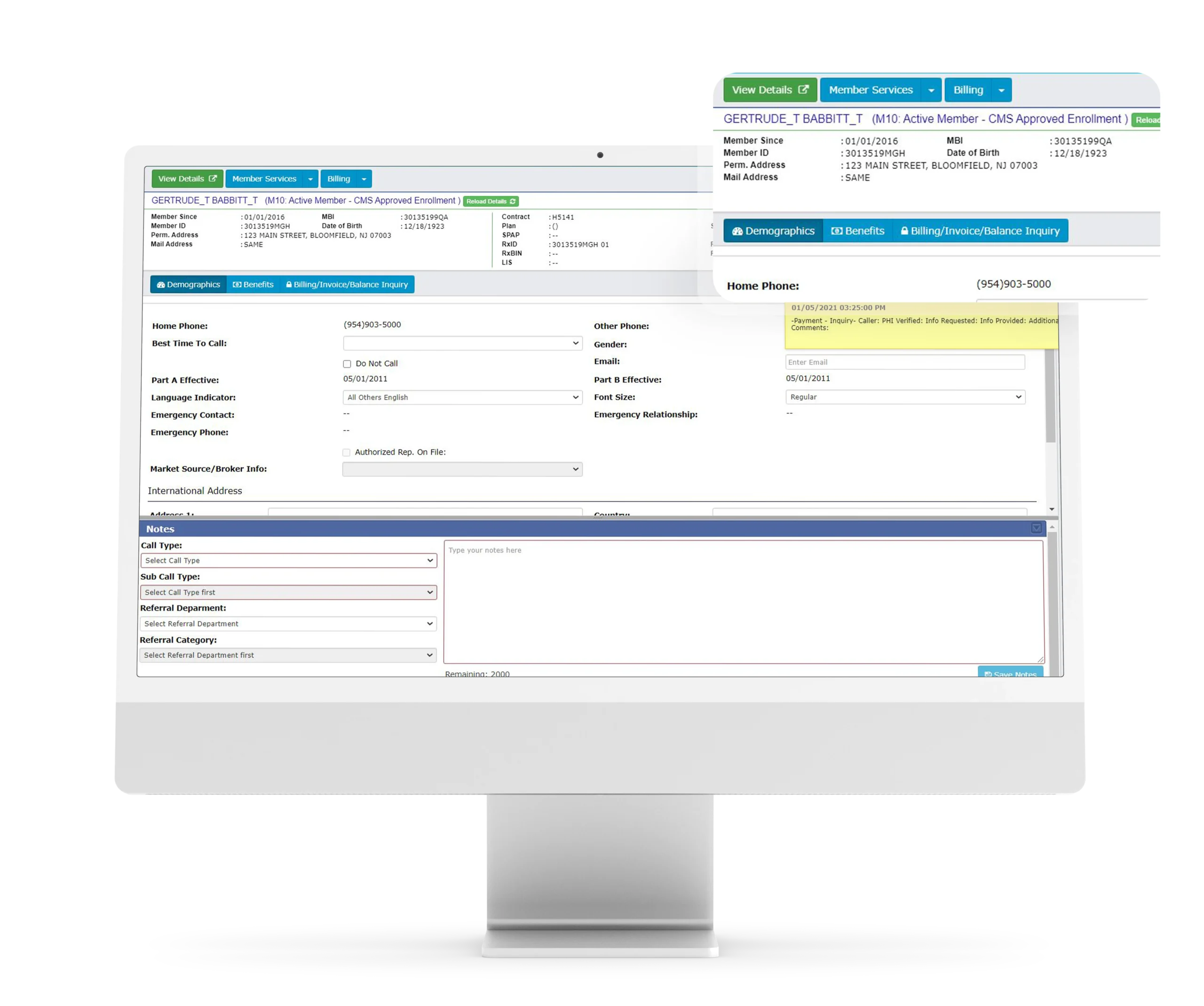
Customer Service
Achieve one-call resolution with the customer experience interface that empowers contact center agents to provide exceptional customer service to your membership.
Access aggregated, pertinent member data–including member-specific action items and alerts automatically reconciled to the member record–for limited screen / system navigation.
Integrations
The Miramar enrollment and billing platform connects key constituents via API.
We integrate seamlessly with CMS and external enrollment portals. Allow us to integrate with your claims processor, pharmacy benefit manager (PBM), financial institution of choice, and more for even faster and efficient communication with your membership.


Deploy a comprehensive platform that supports enrollment, billing, reconciliation, and more. Seamlessly integrate it with your existing platforms and configure any of our solutions to your plan’s needs.
